My MOAS explained
Dave researched his cytoreductive surgery and HIPEC
When you are looking at the diagrams, you’re looking at them as if the person in the diagram is standing up facing you – so the right side is on the left of the diagram.
~ Dave
A midline laparotomy excising the umbilicus
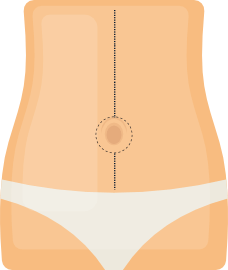
It is the the surgical procedure where the abdomen is cut open to gain access into the abdominal cavity via the abdominal wall. This procedure is also known as a celiotomy. The laparotomy is the first step in the procedure with a midline incision being the most common type of incision which starts at the point where the ribs meet in the centre of the breast down to the pubic bone. These incisions are used as they allow the surgeon a wide access to most of the abdominal cavity giving access to any abdominal organ or space. In my case, my umbilicus (belly button) was also removed which I understand is frequently done with this operation.
The right paracolic gutter was stripped
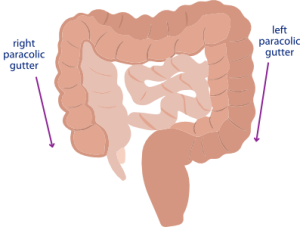
The paracolic gutters (paracolic sulci, paracolic recesses) form spaces between the colon and the abdominal wall. There are two paracolic gutters; the right lateral paracolic gutter and the left lateral paracolic gutter. They play important roles in the abdominal cavity as they allow a passage for infectious fluids from different areas of the abdomen. For example, most occurrences of PMP start at the appendix and can result in the appendix perforating.
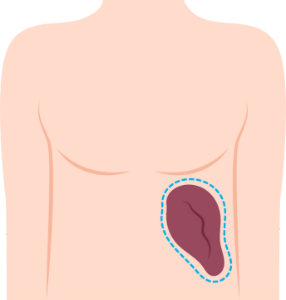
A right hemicolectomy
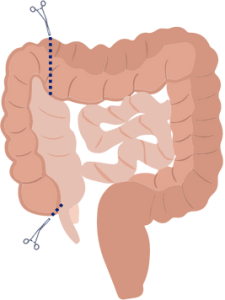
The ascending colon is referred to as the right and the descending colon is referred to as the left. The transverse colon runs across the top joining the left and right together and when this is resected it is referred to as an extended hemicolectomy.
Stripped the left diaphragm and mobilised up the spleen
The diaphragm is a muscle that separates the chest from the abdomen and plays a crucial role in breathing. Stripping the left diaphragm involves removing any tumour growth that may have spread to this area. The surgeon will carefully separate the diaphragm from surrounding tissues and remove any tumour growth. The left diaphragm is particularly important to remove as it provides a pathway for tumours to spread from the abdomen to the chest.
The spleen sits in the upper left side of the abdomen and is approximately the size of your fist. The spleen plays a number of roles in the human body including the filtering of blood in support of the immune system. It recycles red blood cells and stores platelets and white blood cells. It also helps to fight off a number of bacteria. Approximately 10% of people have a second “accessory spleen”!
Mobilising up the spleen involves carefully detaching the spleen from its surrounding tissues and moving it upwards. This helps to provide better access to the back of the abdomen, allowing the surgeon to remove any tumour growth from this area. At this point the spleen is mobilised prior to the removal of the omentum and the eventual removal of the spleen itself.
The spleen is particulary particularly helpful in fighting pneumococcus, meningococcus and hemophilus. As such, you may be advised to have vaccinations before your surgery.
A greater omenectomy taking the gastroepiploic vessels off the stomach
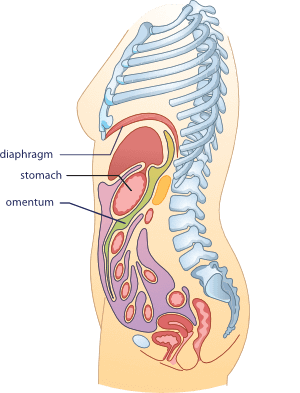
So, the greater omentum is basically this large, sheet-like fold of tissue that hangs down from the stomach. It kind of looks like an apron that covers the intestines. This tissue passes in front of the small intestines and then moves upward to reach the back wall of the abdomen, crossing over the transverse colon as it goes.
The omentum is a really interesting piece of tissue. It’s mostly used for storing fat, but it also helps out the immune system. Inside the omentum, there are these special cells called macrophages that can gobble up any bad bacteria or viruses that might be hanging around in your body. It’s also pretty cool that the omentum can wrap itself around an infected or wounded area to help protect it.
Scientists think that the omentum also plays an important role in keeping our internal environment healthy, but it’s not like we can’t live without it or anything like that. It’s definitely not an essential organ like your heart or your lungs, but it’s still pretty neat!
During cytoreductive surgery, the surgeon may perform a greater omentectomy by taking the gastroepiploic vessels off the stomach. The gastroepiploic vessels are blood vessels that supply the greater omentum and the stomach. The pronunciation of gastroepiploic is gas-troh-ep-uh-ploh-ik. By taking these vessels off the stomach, the surgeon can remove the greater omentum and any cancerous tissue that may be present.
Removing the greater omentum may be necessary in cases where the cancer has spread to this area or to prevent the spread of cancer to the omentum. It is also sometimes performed as part of a prophylactic surgery in patients at high risk of developing abdominal cancers.
Removed the spleen and omentum
In cytoreductive surgery, removing the spleen and omentum is a common procedure that can help treat advanced PMP and related cancers. The spleen is an organ located in the upper left side of the abdomen, while the omentum is a large fold of tissue that hangs down from the stomach.
The spleen helps filter and clean your blood, makes some new blood cells, and stores extra blood. It’s a pretty important organ, but you can live without it if necessary (although you might be at higher risk for certain infections).
The omentum is a fold of tissue that stores fat, helps fight infection, promotes tissue repair, and may play a role in metabolism. It’s a pretty interesting organ.
Removing the spleen is sometimes necessary when cancer has spread to this organ or if it needs to be removed to gain access to other organs for surgical treatment. The omentum, on the other hand, may be removed as a precaution or if cancer has spread to this area.
When both the spleen and the omentum are removed, it can help to remove a significant amount of tumour from the mid-abdomen.
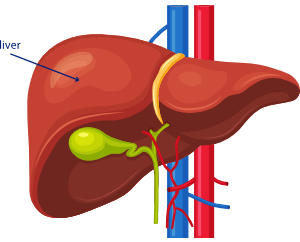
A lesser omentectomy
The lesser omentum is a fold of tissue that connects the liver to the stomach and the duodenum (the first part of the small intestine). It is located in the upper part of the abdomen, behind the liver and the stomach.
It contains important blood vessels, including the hepatic artery, the portal vein, and the bile duct. These vessels help transport blood and nutrients between the liver, the stomach, and the duodenum.
The lesser omentum also plays a role in supporting and stabilizing the organs in the upper part of the abdomen, and it can act as a barrier to prevent the spread of infections between different parts of the abdomen.
A lesser omentectomy is a surgical procedure that is sometimes performed as part of cytoreductive surgery to treat PMP. This is done in order to remove any cancerous tissue that may be present in this area, as the lesser omentum can sometimes be affected by PMP.
Removing the lesser omentum can be challenging, as it is located near several other important organs, including the liver, stomach, and pancreas. As a result, this procedure is usually performed by highly skilled surgical teams with expertise in cytoreductive surgery.
Stripped the porta-hepatis and did a cholecystectomy transfixing the cystic ducts and cystic artery
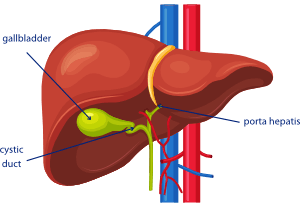
The porta hepatis (also known as the transverse fissure of the liver) is an area located on the underside of the liver where the blood vessels, bile ducts, and lymphatic vessels enter and exit the liver. Stripping the porta-hepatis involves carefully removing any cancerous tissue that may be present in this area. This is done to ensure that all cancerous tissue is removed from the liver and surrounding structures, as the porta-hepatis can be a common site of PMP.
A cholecystectomy is a surgical procedure to remove the gallbladder, which is a small sac located under the liver that stores bile. Transfixing the cystic ducts and cystic artery involves clamping and cutting these structures in order to remove the gallbladder.
The gallbladder’s main function is to store and concentrate bile, which is a fluid produced by the liver that helps with the digestion of fats.
When we eat a meal that contains fat, the gallbladder contracts and releases bile into the small intestine through a duct called the common bile duct. Bile helps break down fats into smaller particles that can be easily absorbed by the body.
The gallbladder also plays a role in the regulation of bile production. It can absorb excess water from the bile to make it more concentrated, and it can release stored bile into the small intestine as needed.
While the gallbladder is an important organ for the digestion of fats, it is not essential for life. People can live without a gallbladder, although they may experience some digestive changes and need to make adjustments to their diet.
Next, the surgeon carefully stitched the cystic duct, which connects the gallbladder to the common bile duct, and the cystic artery, which supplies oxygenated blood to the gallbladder and cystic duct. This process is called suturing, and it ensures that these structures are securely closed off and won’t cause any problems later on. In medical terms, this is also known as “transfixing” the cystic duct and artery.
A diathermy liver capsulectomy with high power diathermy
Removing the liver capsule can help the surgeon to access and remove any tumours that may be attached to the surface of the liver. This can be important for achieving a complete cytoreduction, which means removing as much of the cancer as possible. The diathermy technique is often used in liver surgery because it can help to minimize blood loss and ensure precise cutting.
Stripped the left paracolic gutter
See above for the details of paracolic gutters.
A pelvic peritonectomy
The peritoneum is this thin layer that lines most of the organs in your abdomen. It’s like a cozy blanket that provides support and helps carry important stuff like blood vessels, lymph vessels, and nerves. It looks like very thin plastic wrap. The space inside the peritoneum is called the intraperitoneal space.
During a pelvic peritonectomy, the surgeon removes the peritoneum. This may involve removing all or part of the peritoneum in the pelvis, depending on the extent of the cancer.
Removing the peritoneum can be important for achieving a complete cytoreduction, which means removing as much of the cancer as possible. The peritoneum can be a site for cancer spread in PMP, and removing it can help to prevent the cancer from growing or spreading further.
Anterior resection
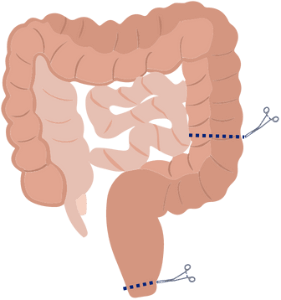
During an anterior resection, the surgeon will remove the affected portion of the colon or rectum, along with any nearby lymph nodes or tissue that may be affected by the disease. The remaining healthy tissue is then reconnected to allow for normal bowel function.
This is called an anastomosis. The surgeon may use either sutures or special staples to make the join. In my case an ileostomy was also performed.
An ileostomy involves creating an opening in the abdomen called a stoma, through which a portion of the small intestine (ileum) is brought to the surface of the skin. This allows waste to bypass the colon and exit the body through the stoma into a specially designed pouch that is worn outside the body.
An ileostomy during cytodreductive surgery for PMP is usually temporary, as was mine. The ileostomy gives the bowel time to recover and heal from the trauma of the operation and can usually be reversed at a later date.
Heated intra operative Mitomycin C at 41 deg C
The last part of the treatment was a special type of chemotherapy called hyperthermic intraperitoneal chemotherapy (or HIPEC for short). Basically, they heated up a special solution of chemotherapy called Mitomycin C to a temperature of 41 degrees Celsius and then put it into my abdomen. The Mitomycin C works by sticking the cancer cells’ DNA together so they can’t grow any more. The surgeon made sure to spread the chemotherapy solution around the whole abdomen to make sure it covered all the cancer cells.
The HIPEC treatment is given to make sure that any tiny bits of cancer that might still be in the body after the surgery are targeted and destroyed. The Mitomycin C, which is the chemotherapy drug used in my treatment, can only penetrate tissues up to a depth of about 2.5mm, which is just enough to reach and target any remaining cancer cells. In fact, doctors use this depth of 2.5mm as a way to define complete cytoreduction – meaning that they have removed all visible signs of cancer during the surgery.
The time the HIPEC is in the abdomen varies by treatment centre and the chemotherapy agent used (30-120 minutes).
Post Op
After the heated chemotherapy treatment was done, the surgical team joined my rectal stump and colon together (anastomosis), completed the ileostomy and closed the wound. After the operation, I received four days of early postoperative intraperitoneal chemotherapy (EPIC). This involved the administration of the chemotherapy solution via drains directly into my abdomen. The infusion took around an hour and the solution was left in for 23 hours before being drained and replaced. During this treatment, I was moved regularly to make sure the solution was evenly distributed throughout my body. I understand that EPIC isn’t commonly used and its value to HIPEC alone or CRS alone is still under debate.
Written: David Mason and Angela Brook
Reviewed: Dr Laura Lambert
Updated: 20th April 2023
References
Early postoperative intraperitoneal chemotherapy (EPIC) following cytoreductive surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC)...
Fung X, Li IC, Chandrakumaran K, et al. Early postoperative intraperitoneal chemotherapy (EPIC) following cytoreductive surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in 632 patients with Pseudomyxoma peritonei of Appendiceal origin: A single institution experience. European Journal of Surgical Oncology. 2022;48(7):1614-1618. doi:10.1016/j.ejso.2022.02.002
Pseudomyxoma peritonei: Natural history and treatment
Mittal R, Chandramohan A, Moran B. Pseudomyxoma peritonei: Natural history and treatment. International Journal of Hyperthermia. 2017;33(5):511-519. doi:10.1080/02656736.2017.1310938
Current trends in cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) for...
Harper MM, Kim J, Pandalai PK. Current trends in cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal disease from Appendiceal and colorectal malignancies. Journal of Clinical Medicine. 2022;11(10):2840. doi:10.3390/jcm11102840
Consensuses and controversies on Pseudomyxoma Peritonei...
Lin Y-L, Xu D-Z, Li X-B, et al. Consensuses and controversies on Pseudomyxoma Peritonei: A review of the published consensus statements and Guidelines. Orphanet Journal of Rare Diseases. 2021;16(1). doi:10.1186/s13023-021-01723-6
Home > Information about pseudomyxoma peritonei (PMP) > The Sugarbaker technique > My MOAS explained > Components of my MOAS