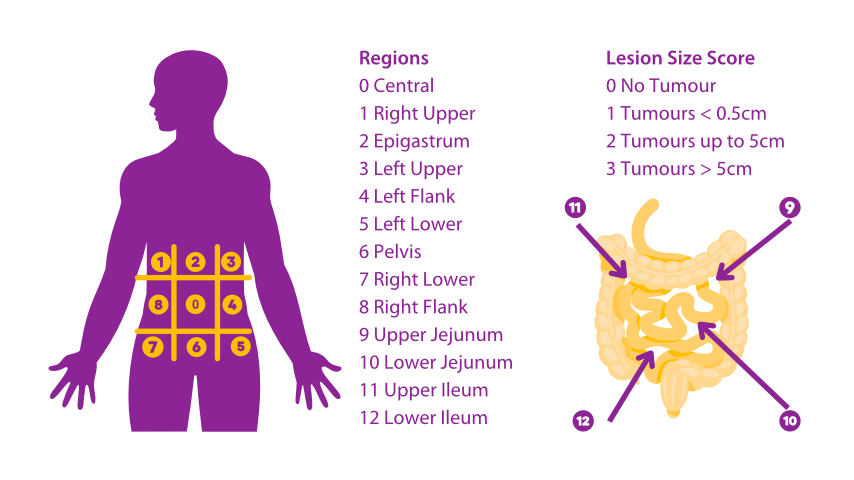
The peritoneal cancer index or PCI score is used to quantify the extent of peritoneal cancer spread for pseudomyxoma peritonei (PMP) and other peritoneal surface malignancies. It provides an objective measure of overall tumour burden to help guide treatment decisions and predict prognosis. The PCI score is also known as the Sugarbaker score after Dr Paul Sugarbaker who devised this quantification.
About the PCI Score
The abdomen and pelvis are divided into 13 regions. Each region is assigned a score of 0 (no tumour), 1 (tumour 1-5 mm), 2 (tumour 5-25 mm), or 3 (tumour >25 mm). Scores are added for each region to get a total PCI.
A lower PCI, around 10-20, indicates limited disease spread and is associated with a better prognosis. These patients are optimal candidates for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS/HIPEC).
A PCI of 20-30 still represents potentially resectable disease for some patients. Neoadjuvant chemotherapy may be used before CRS/HIPEC to help shrink the tumour volume. Outcomes begin to decrease more rapidly above a PCI of 25.
A PCI above 30-40 typically means the cancer has spread too extensively throughout the peritoneum to be fully resected surgically. Palliative management focusing on symptom relief usually provides the best option at this point rather than cure-directed treatment.
Some studies use PCI categories of: 0-10 (very limited), 10-20 (limited), 20-30 (moderate), and over 30 (extensive). These provide a simplified way of stratifying patients into prognosis groups to help guide treatment decisions and set goals.
Changes in PCI over the course of treatment and follow-up indicate how well the cancer is being controlled. A declining PCI shows the therapy is working, while a rising PCI suggests progressive disease and treatment failure. Close monitoring PCI is used to detect recurrence early.
Retreatment like repeat CRS/HIPEC may be options if PCI increases after initial definitive treatment but still remains within a potentially resectable range, especially if good response was seen initially. Multiple procedures are sometimes needed over the course of management and survivorship.
The PCI correlates with other factors impacting prognosis like tumour grade, lymph node involvement, organ involvement, and patient health. But it provides a simple objective measure of bulk tumour burden that directly influences treatment recommendationsand options.
There is ongoing research to further improve the PCI scale, develop alternative scoring systems, and raise minimally acceptable standards to continue advancing Treatment of PMP and peritoneal malignancies. The goal is enabling lower PCI scores and complete cytoreduction for higher percentages of appropriately selected patients.
In summary, the PCI score is essential for guiding management decisions at all stages of PMP and other peritoneal surface malignancies. It provides critical information to help determine prognosis, set treatment goals, select between options, plan surgeries, monitor response, and guide further management if the disease recurs. By objectively quantifying tumour extent, the PCI improves the standardization and evidence-base behind decision making for these rare peritoneal surface malignancies.
More FAQs
What is HIPEC surgery?
HIPEC is a cancer treatment that involves surgery and heated chemotherapy. It’s used for advanced abdominal cancers like pseudomyxoma peritonei.
Will exercising cause pseudomyxoma peritonei (PMP) to spread?
Engaging in exercise is generally beneficial for overall health and well-being, even for individuals with pseudomyxoma peritonei (PMP). Exercise can help improve cardiovascular fitness, strengthen muscles, boost immune function, enhance mood, and promote a sense of...
Why is HIPEC controversial?
Some doctors still view HIPEC (hyperthermic intraperitoneal chemotherapy) as a controversial procedure for multiple reasons.
References
Clinical research methodologies in diagnosis and staging of patients...
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treatment and Research. 1996:359-374. doi:10.1007/978-1-4613-1247-5_23
Peritoneal carcinomatosis: Cytoreductive surgery and HIPEC...
Brücher BLDM, Piso P, Verwaal V, et al. Peritoneal carcinomatosis: Cytoreductive surgery and HIPEC–-overview and Basics. Cancer Investigation. 2012;30(3):209-224. doi:10.3109/07357907.2012.654871