What is
pathology?
Information about PMP
Most people think of autopsies when pathology is mentioned, but post mortem examinations are only part of pathology.
In fact, the majority of pathologists are based in hospitals and deal with specimens from living patients. The branch of pathology in which surgical specimens are examined under the microscope is called histopathology.
We’re going to discuss the role of histopathology in diagnosis and treatment of pseudomyxoma peritonei (PMP) and the appendiceal tumours that are the most common cause.
What happens to a surgical specimen in the histopathology laboratory?
When the surgeon has removed an organ from the body, it is normally placed in a solution of formalin that preserves it and prevents decomposition. This is called fixing the specimen.
The specimen is sent to the histopathology laboratory where it is dissected by a pathologist or trained biomedical scientist.
The aim of specimen dissection is to:
- Record and describe the organs or other material received.
- Look for any features that may be important in prognosis or treatment (for example, in the appendix this might include whether the wall has ruptured)
- Select pieces of tissue for examination under the microscope
PMP isn’t like other types of cancer as it seldom spreads through the bloodstream or lymphatic system. It stays contained within the abdomen where it spreads along the inner surfaces, spread by the mucin. It isn’t currently known what causes PMP. The name ‘pseudomyxoma peritonei’ means “false mucinous tumour of the peritoneum”; the peritoneum is another name for your abdominal cavity.
For examination under the microscope
The selected tissue samples are embedded in a paraffin wax (similar to the wax used to make candles), which allows very thin sections to be cut.
The pieces of tissue are usually about 2cm wide and the sections are about 4μm thick. A human hair is about 20 times thicker. The thin sections are stained so that the cells become visible under the microscope. The ones used most commonly in the histopathology lab are dyes and immunohistochemical stains.
The slides are examined by a pathologist. Pathologists are medically qualified doctors who specialise in this field. The pathologist’s report is sent to the surgeon and makes an important contribution to management
decisions.
For example, the report will usually include:
- The diagnosis
- Features that can guide further treatment
- Features that may point to the likely outcome (prognosis)
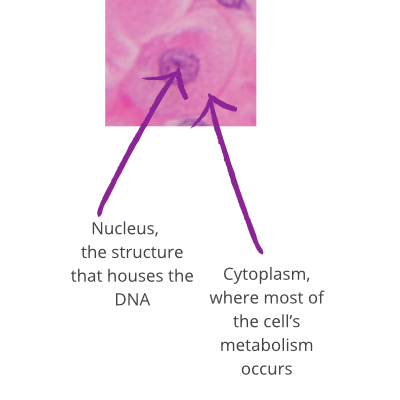
A dye stain
Dyes stain the cells different colours. The image shows a cell with the combined haematoxylin and eosin stain. Haematoxylin is blue and eosin is pink/red.
An immunohistochemical stain
Immunohistochemistry specifically identifies individual substances in the specimen. These stains use antibodies that only react with one particular substance. For example, the image shows a cancer in which immunohistochemistry for CEA (a marker of certain types of tumour) is positive.
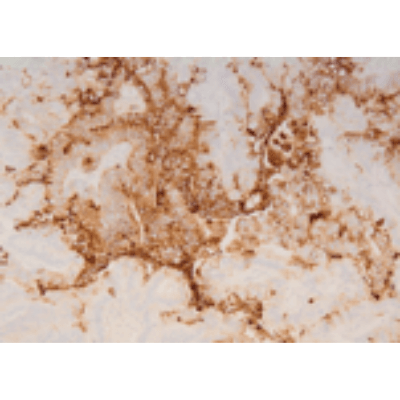
The brown colour is the positive reaction and confirms the presence of CEA in the cancer.
I found out I had an appendix tumour during my c-section
I developed an umbilical hernia and when it was being repaired they found the mucin. Only with follow up tests they found the root cause.
I’m now on ‘watch and wait’ following a diagnosis of pseudomyxoma peritonei.
For me, it all started with blood in my urine and an increase in the size of my stomach. In retrospect, I could feel the mucin moving when I walked.
What do those abbreviations mean?
It’s totally normal to feel overwhelmed with all the new medical jargon you’re hearing. Our glossary has got your back! It’s a handy tool to quickly find what different terms mean, so you can focus on understanding your diagnosis without getting lost in the details.
References
The pathology of pseudomyxoma peritonei and appendix tumours
Pseudomyxoma Survivor and N Carr, MB BS FRCPath FRCPA FAcadMEd, Pseudomyxoma Survivor website, 2023
A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia
Carr, Norman J. FRCPath; Cecil, Thomas D. MD; Mohamed, Faheez; Sobin, Leslie H.; Sugarbaker, Paul H.; González-Moreno, Santiago MD PhD; Taflampas, Panos MD; Chapman, Sara PhD; Moran, Brendan J. MD, A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia, The American Journal of Surgical Pathology: January 2016 – Volume 40 – Issue 1 – p 14-26 doi: 10.1097/PAS.0000000000000535
This Toggle Intentionally Left Blank
Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique)
National Institute for Health and Care Excellence (NICE) Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique), April 2004 [Online]. Available https://www.nice.org.uk/Guidance/ipg56 [Accessed February 2018]. Under review February 2018.
Pseudomyxoma peritonei
Cancer Research UK, Pseudomyxoma peritonei, 2016 [Online]. Available http://www.cancerresearchuk.org/about-cancer/pseudomyxoma-peritonei [Accessed February 2018].
Pseudomyxoma peritonei (PMP)
Macmillan, Pseudomyxoma peritonei (PMP), 2016 [Online]. Available https://www.macmillan.org.uk/information-and-support/pseudomyxoma-peritonei-pmp [Accessed February 2018].