According to the National Institute for Health and Care Excellence (NICE), the Sugarbaker technique was developed by Dr Paul Hendrick Sugarbaker at the Washington Cancer Institute. It involves complete surgical tumour removal (also known as complete cytoreduction) combined with intraoperative heated chemotherapy (HIPEC). The operation takes about 10 hours to complete and may include:
- removal of the right hemicolon, spleen, gallbladder, greater omentum and lesser omentum
- stripping of the peritoneum from the pelvis and diaphragm
- stripping of tumour from the surface of the liver
- removal of the uterus and ovaries in women
- removal of the rectum in some cases
As a patient with pseudomyxoma peritonei or appendix cancer, your doctor will do their best to explain to you the impact this disease will have on you and any proposed treatments or surgeries.
It may be very hard for you to understand the impact that any treatment might have on you. It’s very easy to assume that every organ we have is essential and that its absence will impact our quality of life profoundly. In fact, many organs serve only a limited purpose nowadays – for example, our gallbladder plays an important role in digesting large amounts of fat. If you were a caveman, eating a woolly mammoth along with your family, unsure when you would next eat, this is important. Nowadays, it serves only a peripheral role in digestion (as long as you go easy at the barbecue!). Of course other organs still perform important roles, but we can manage without all or some parts of them. We’re going to take a look in layman’s terms where each organ is. We’ll also have a look at the role they play and the impact on your quality of life would be, should your doctor suggest removal.
Sounds great but what does it mean, where are all these organs, what do they do and how can you manage without them? You can click on any of the images to see it enlarged.
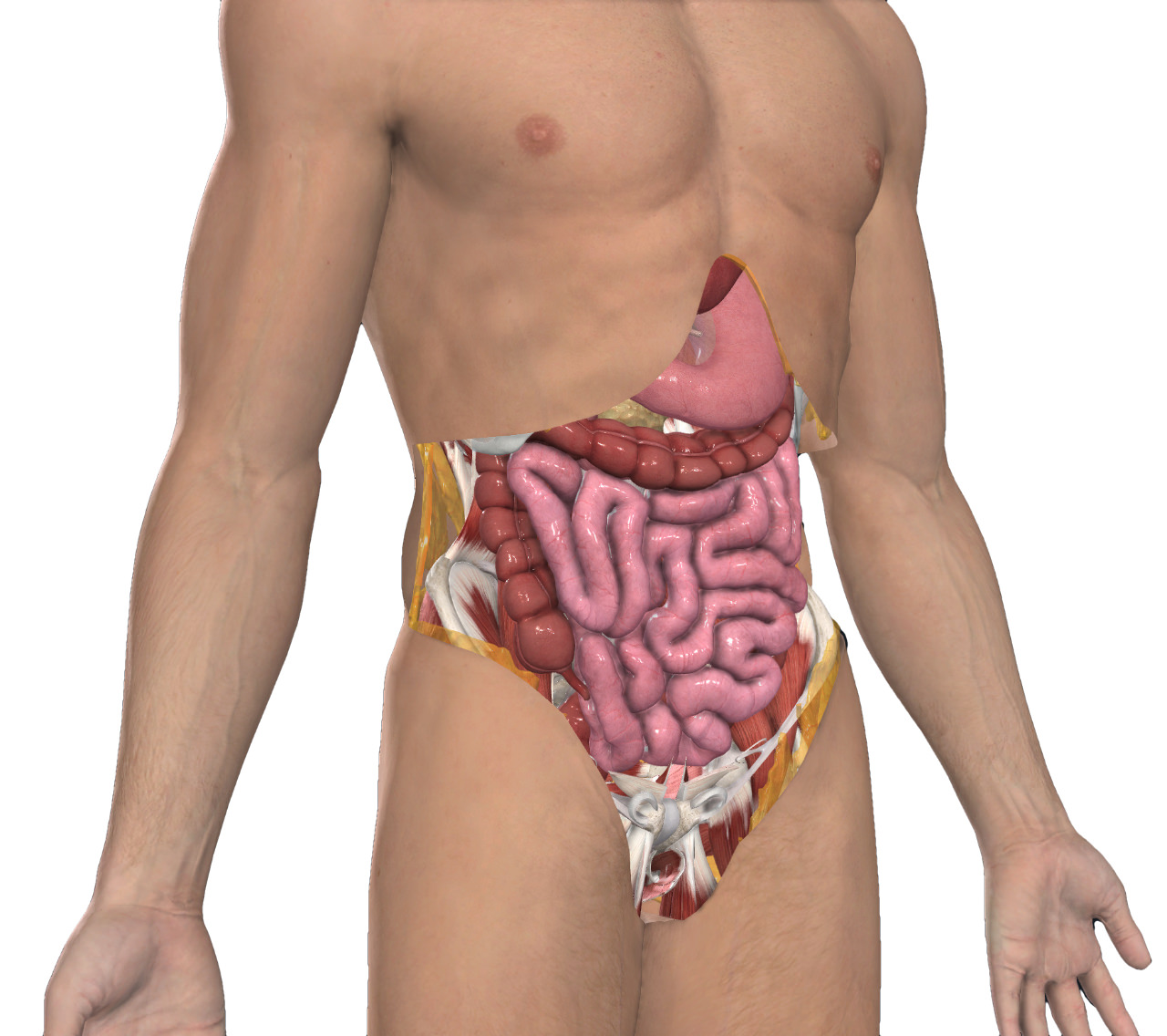
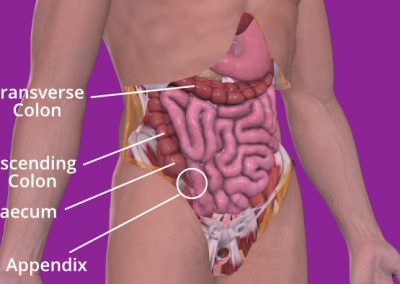
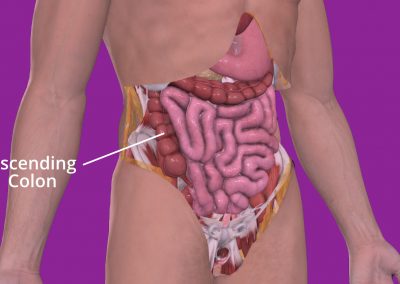
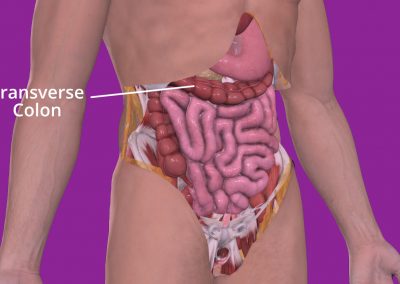
Removal of the right hemicolon
The colon is the large tube-like part of your digestive system that comes after the small bowel. It goes down to your bottom where it connects to the rectum and anus. When you have surgery to remove the right side of your colon, it’s called a right hemicolectomy. This means the surgeon will remove your appendix, caecum, ascending colon, and a bit of your transverse colon.
The caecum is a small pouch that connects your small and large intestines. Your appendix is attached to it. The ascending colon goes upwards toward the liver, while the transverse colon goes across your belly from the ascending colon and loops under your spleen. Usually, this much of your colon is removed during surgery, not because of the disease spreading, but because the colon’s blood supply is structured this way.
If you have surgery to remove a part of your colon, you might not notice much difference in how you digest food. But sometimes people might have stomach pains or diarrhoea. If you have these symptoms, your doctor might suggest you drink more water and eat certain foods to help your body control your bowel movements. It’s important to talk to your doctor if you have any stomach pain or diarrhoea after the surgery.
After having your caecum removed, you may experience some changes in your digestion. This is because the caecum and the appendix play a role in the absorption of fluids and salts from the digestive tract. You may need to make some dietary changes to help manage any symptoms you experience after surgery. Your doctor or a dietitian can give you advice on what foods to eat and avoid. It’s important to follow your doctor’s instructions and attend follow-up appointments to monitor your recovery.
Removal of the spleen
Sitting next to your pancreas and stomach, behind your left ribs, your spleen is basically a fist-sized, large-scale factory for controlling the number of blood cells in your body, filtering the blood and fighting germs. As such, it has large, important blood vessels which route to and from it and so injury of the spleen can be significant.
If you have had your spleen removed, you will be more likely to catch certain infections, especially those caused by bacteria. Therefore, you will need to take extra care to avoid getting infections.
Other parts of your body, such as your liver, can also make and store blood cells and can fight infection. The loss of your spleen only becomes important when you are critically ill in fighting off an infection, or suffering from significant injury, where those stored blood cells become relevant.
If it is planned for you to have your spleen removed, your doctor might recommend that you get certain vaccinations to help protect you. Additionally, you might need to take antibiotics before some medical procedures or before travelling to certain countries. This is because having your spleen removed weakens your immune system and can make you more likely to get an infection. The NHS website has further details on the vaccinations you should have.
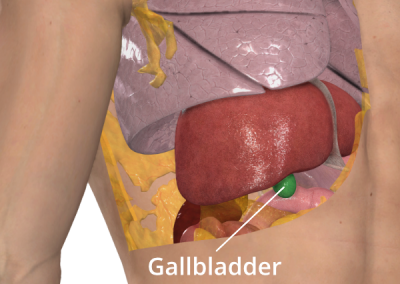
Gallbladder
The gallbladder is a small organ located in the upper right side of the abdomen, just below the liver. Its main function is to store and release bile, a digestive fluid produced by the liver that helps the body digest fats in the small intestine. The gallbladder releases bile into the small intestine through a duct called the common bile duct. The gallbladder isn’t essential for life, and you can live without one if it needs to be removed.
The removal of your gallbladder is called a cholecystectomy (koh-luh-sis-TEK-tuh-me).
If your gallbladder has been removed, you may need to make some dietary changes to help your body digest fats. Without the gallbladder, bile may be released less efficiently, leading to difficulty in digesting fats. Speak to your doctor is this is a concern for you.
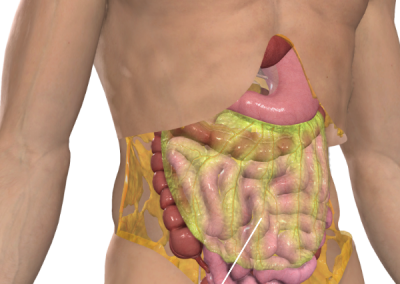
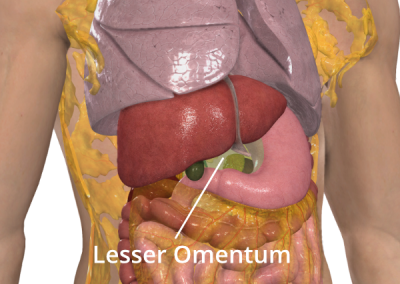
Greater and lesser omentum
The omentum is a layer of fatty tissue comes in two parts, the greater and lesser omentum. These are a pair of ‘curtains’ which overlay your lower abdomen, primarily your small and large intestines. The greater omentum is over the front, like an apron, from the bottom curve of your stomach with the the lesser omentum going upwards from the inner curve of your stomach.
As with many structures in the body, they serve more than one function. Primarily, they help your intestines and other organs to remain static within your abdomen even when you are undertaking extreme motions such as athletics. Like all curtains, the omenta have folds which interleave the organs and keep them broadly in place. A secondary function of the omenta is to serve a role in the immune system, helping to fight infection.
If these tissues are partially or completely removed, it may cause some changes in your digestion and bowel function. You may need to make adjustments to your diet, such as eating smaller and more frequent meals, avoiding fatty and spicy foods. Additionally, your doctor may recommend medications to help with digestion or to manage any symptoms you may experience. It’s important to follow your doctor’s instructions and attend any follow-up appointments to ensure proper healing and management of any potential issues.
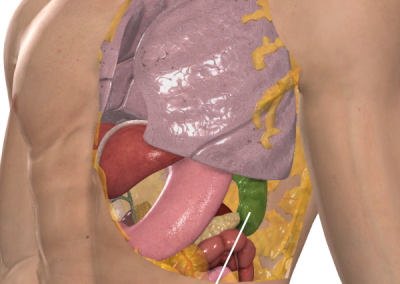
Peritoneum
The peritoneum is a thin, transparent membrane that lines the abdominal cavity and covers the organs within it, including the stomach, intestines, liver, spleen, and ovaries. It acts as a protective layer that helps to reduce friction between the organs and the abdominal wall and helps to keep the organs in place. The peritoneum also plays a role in the absorption and transport of nutrients and waste products between the organs and the bloodstream.
The name for the surgical procedure to remove part or all of the peritoneum is a peritonectomy. It is pronounced as “peh-rih-tuh-NEK-tuh-mee“.
Stripping of the peritoneum from the pelvis and diaphragm is a major surgical procedure in itself and is typically done to treat certain types of cancer. If you have this procedure it is likely that you would experience some pain and discomfort in the area. There may also be some changes in your bowel and bladder function, as well as temporary swelling and bruising in the abdomen. It’s important for you to follow your doctor’s instructions carefully, including taking any prescribed medications and avoiding certain activities until healed sufficiently.
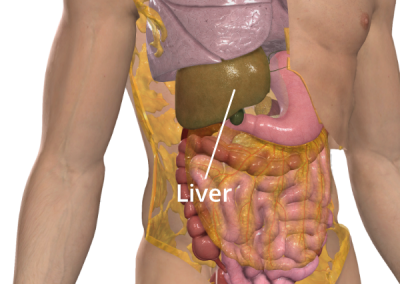
Stripping of tumour from the surface of the liver
The liver is like a really cool factory in your body! It makes a lot of important things your body needs. For example, it turns the sugar from your favorite Mars Bar into a type of sugar called glucose that your body uses for energy. The liver also makes something called bile salts that help your body digest food.
Pseudomyxoma peritonei can cause tumours on the surface of your liver. While you can’t live without your liver, doctors can remove these surface tumours by “scrubbing” them off. They can also remove parts of the liver if needed without harming you. Another way to remove surface tumours is through a procedure called a liver capsulectomy. Your liver is surrounded by a tissue capsule that can be removed without harming you, and this will also remove any surface tumours. If necessary, diathermy can be used. This is when heat is used to destroy the tumours that are sticking to the surface of the liver.
The surgical procedure that involves the removal of a capsule of tissue surrounding an organ, such as the liver, is called a capsulectomy. The term is pronounced “kap-suh-LEK-tuh-mee“.
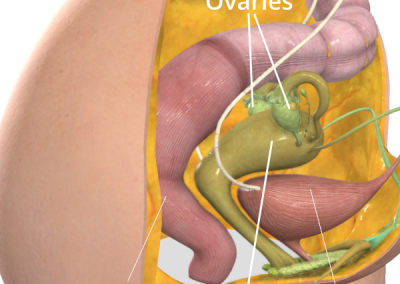
Removal of the uterus and ovaries in women
The uterus is a part of a woman’s body that is also called the womb. There are special tubes called the fallopian tubes that allow eggs to travel from the ovaries to the uterus. If a woman has a partner and their egg meets a sperm in the uterus, it can grow into a baby.
Sometimes, doctors need to remove the ovaries, womb, or fallopian tubes. If they do, it can make it hard or impossible for a woman to have a baby. If the ovaries are removed, it can also make women enter the menopause right away. This can make women feel uncomfortable or have hot flushes. There is medication called hormone replacement therapy (HRT) that can help with these symptoms.
The removal of the womb is called a sub-total hysterectomy (hiss-ter-ek-tuh-mee). The removal of the womb and cervix is named a total hysterectomy. Salpingectomy (sal-ping-EK-tuh-me) is the name given to the removal of a fallopian tube. Oophorectomy (oh-uh-fuh-REK-tuh-mee) is the name given to the removal of an ovary. So a total hysterectomy with bilateral salpingo-oophorectomy is the removal of the womb, cervix, fallopian tubes and ovaries. It’s pronounced toh-tl his-tuh-rek-tuh-mee wihth by-luh-tuh-rul sal-ping-go oh-fuh-rek-tuh-mee.
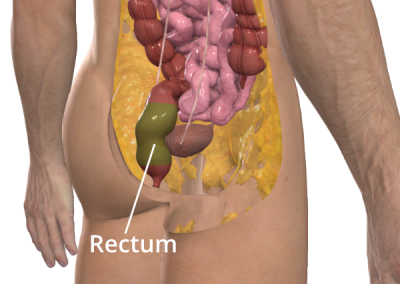
Removal of the rectum in some cases
The rectum is the last part of the large intestine or colon. It connects the colon to the anus and stores stool until it is ready to be passed out of the body during a bowel movement. When the rectum is full, it sends signals to the brain that it’s time to go. When you go to the toilet, the muscle around the anus relaxes to let the poop out of the body.
The surgical name for the removal of the rectum is called a proctectomy. It is pronounced as prok-TEK-tuh-mee.
Losing your rectum means that you will have to make some changes in your daily life to keep yourself healthy and comfortable. Since the rectum is the last part of the large intestine, it’s important to be mindful of what you eat to avoid constipation or diarrhoea. You may need to take medications or use special techniques to help you go to the bathroom. It’s important to talk to your doctor about any concerns or questions you have about living without a rectum.
Images courtesy of 3D4Medical, with permission.
Dave's cytoreductive surgery and HIPEC explained
Dave’s study of the components of his cytoreductive surgery and heated intraperitoneal chemotheraphy (CRS/HIPEC) provides a unique perspective on what it’s like to undergo these procedures. Like many patients, Dave was curious about what would happen during his surgery and wanted to better understand the process. His study of these procedures was a real eye-opener, and gave him a newfound appreciation for the surgical teams who perform them. Dave was amazed by the skill and dedication of the surgical team, and the incredible resilience of the human body in the face of such radical surgery. His experience highlights the importance of education and understanding when it comes to these complex procedures. By taking the time to learn more about cytoreductive surgery and HIPEC, patients like Dave can better prepare themselves for what to expect and have a greater appreciation for the remarkable work of their surgical teams.
References
Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique)
NICE (2004, April 28). Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique). Retrieved February 28, 2023, from https://www.nice.org.uk/guidance/ipg56
Cytoreductive Surgery and Perioperative Intraperitoneal Chemotherapy as a Curative Approach to Pseudomyxoma Peritonei Syndrome
Sugarbaker PH (2001). Cytoreductive Surgery and Perioperative Intraperitoneal Chemotherapy as a Curative Approach to Pseudomyxoma Peritonei Syndrome. Sage Journals. Published July 2001. Retrieved March 7, 2023, from doi:10.1177/030089160108700415
Right Hemicolectomy
ACPGBI. Right Hemicolectomy. The Association of Coloproctology of Great Britain and Ireland (ACPGBI). Retrieved March 21, 2023, from https://www.acpgbi.org.uk/patients/procedures/5/right_hemicolectomy/
Spleen problems and spleen removal
NHS. Spleen problems and spleen removal. NHS Website for England. Retrieved March 21, 2023, from https://www.nhs.uk/conditions/spleen-problems-and-spleen-removal/
Cholecystectomy (gallbladder removal)
Mayo Clinic. Cholecystectomy (gallbladder removal). Retrieved March 21, 2023, from https://www.mayoclinic.org/tests-procedures/cholecystectomy/about/pac-20384818
Incidental Diagnosis of Pseudomyxoma Peritonei After Emergent Splenectomy
A rare case of pseudomyxoma peritonei presenting an unusual inguinal hernia and splenic metastasis
Appendiceal pseudomyxoma peritonei: Unmasking the indolent invader
Jain, A., FRACS, Flood, M. P., MRCS, Ramsay, R., PHD, Michael, M., MD, FRACP, Kong, J. C., MBChB, FRACS, MS, PhD, & Heriot, A. G., MD, MBA, FRACS (2022). Appendiceal pseudomyxoma peritonei: Unmasking the indolent invader. ANZ Journal of Surgery,, 92(12), 3135-313. https://doi.org/10.1111/ans.17971
Home > Information about pseudomyxoma peritonei (PMP) > The Sugarbaker technique