What does it mean?
It’s bewildering, so many new words and terms to understand and even worse to try and remember
A-C
abdominal hernia
Adenocarcinoma
Adenocarcinoma is a type of cancer that starts in the glandular cells that produce and secrete fluids such as mucus, hormones, or digestive enzymes. These glandular cells can be found in many parts of the body such as the appendix and colon. These tumours can grow and spread to other parts of the body if not treated.
Appendiceal adenocarcinoma is a rare type of cancer that originates in the lining of the appendix. In the case of appendiceal adenocarcinomas, these cells produce mucus, which can accumulate and cause a condition called pseudomyxoma peritonei. Symptoms of this condition may include abdominal pain and swelling, as well as digestive problems. Treatment for appendiceal adenocarcinoma may involve surgery to remove the appendix and any affected tissue, as well as chemotherapy and other therapies.
It is pronounced a-duh-now-kaa-suh-now-muh.
Adenoma
An adenoma is a type of tumour. An adenoma of the appendix grows within the appendix and then breaks out through the appendix wall. The appendix may reseal afterwards. Whilst the adenoma itself may be benign, the condition is still fatal is left untreated.
The definition of an adenoma is a benign tumour of epithelial tissue with glandular origin, glandular characteristics, or both. Although not common, this type of tumour can become malignant.
Adhesions
Surgical adhesions are bands of scar tissue that form between organs or tissues inside the body after abdominal surgery. These adhesions can cause organs or tissues to stick together, which can lead to pain, discomfort, bowel obstruction, or infertility. Surgical adhesions can occur after any type of abdominal surgery, including surgeries for pseudomyxoma peritonei.
Adjuvant chemotherapy
Adjuvant chemotherapy refers to the treatment given to a person after the primary treatment, such as surgery, in order to prevent the cancer from returning. This chemotherapy is used to kill any remaining cancer cells that may have been left behind after the primary treatment. Adjuvant chemotherapy can also be used to reduce the risk of cancer recurrence and improve a person’s chances of survival.
Asplenia
Asplenia is a condition in which a person is born without a spleen, has had their spleen removed, or their spleen does not work properly. The spleen is an important part of the body’s immune system, which helps fight infections. Without a working spleen, the body may have a harder time fighting certain infections, especially from bacteria that can cause pneumonia or meningitis. It is important for people with asplenia to take special precautions to protect themselves from these infections, such as getting certain vaccinations and taking antibiotics when needed.
Benign
The term “benign” is used in medicine to describe a condition or tumour that is not cancerous and will not spread to other parts of the body. Benign conditions may still cause symptoms or problems and require treatment, but they are not generally life-threatening like cancer.
CA-125
Related to mucin production and generally associated with ovarian cancer and gastrointestinal cancers, CA-125 is a protein often found on the surface of ovarian cancer cells and in some normal tissues.
It is used as a marker for ovarian cancer as well as for PMP. However, CA -25 levels may also be high in other types of non-cancerous conditions, including menstruation, pregnancy and pelvic inflammatory disease.
CA 19-9
Cancer antigen 19-9 (CA 19-9) is a protein that exists on the surface of certain cells. CA 19-9 does not cause cancer; rather, it is a protein that is produced by the tumour cells, making it useful as a tumour marker to follow the course of the cancer.
CA 19-9 is elevated in most patients with pseudomyxoma peritonei and advanced pancreatic cancer, but may also be elevated in other cancers and diseases such as bowel cancer, lung cancer and gall bladder cancer, as well as in benign diseases such as gall stones, pancreatitis, cystic fibrosis, and liver disease. Because elevated levels of CA 19-9 are seen in many diseases, elevated levels do not necessary mean the presence of pancreatic cancer. Very small amounts of CA19-9 may also be found in healthy patients.
Cancer
Cancer is a disease that occurs when the body’s cells start to grow and multiply uncontrollably, leading to the formation of abnormal masses of tissue called tumours. These tumours can be benign, meaning they are not cancerous and do not spread to other parts of the body, or they can be malignant, meaning they are cancerous and can spread to other parts of the body through the bloodstream or lymphatic system. Pseudomyxoma peritonei (PMP) behaves differently.
Cancer fatigue
Cancer-related fatigue is a feeling of extreme tiredness and exhaustion that often affects people with cancer. It is different from regular tiredness or feeling sleepy, and it can last for long periods of time even with rest.
Capecitabine
Capecitabine (brand name: Xeloda) is a chemotherapy medication used to treat various types of cancer, including appendix and colon cancers. It works by interfering with the growth and spread of cancer cells in the body.
Capecitabine is a prodrug, which means that it is converted into its active form inside the body. Once it is taken orally, the drug is absorbed in the small intestine, where it is converted into 5-fluorouracil (5-FU), the active drug. 5-FU is an antimetabolite, which means that it interferes with the growth of cancer cells by disrupting the production of DNA and RNA.
Capecitabine is usually taken twice a day with food, and the dosage depends on various factors, such as the type of cancer being treated, the patient’s weight, and their overall health. It can cause side effects, such as nausea, vomiting, diarrhea, fatigue, and skin rashes. It is important to follow the instructions of the healthcare provider and report any side effects that occur.
Capsulectomy
A capsulectomy is a surgical procedure that involves the removal of a capsule of tissue surrounding an organ, such as the liver. This procedure is often used to remove surface attached tumours from the liver, which may have developed due to conditions such as cancer. The term is pronounced “kap-suh-lek-tuh-mee“.
Capsule Endoscopy
A capsule endoscopy is a non-invasive medical procedure used to examine the inside of the small intestine. It involves swallowing a small, disposable capsule containing a tiny camera, a light source, and a transmitter. The capsule is about the size of a large pill and is designed to move through the digestive system naturally, without causing any discomfort or disruption.
As the capsule travels through the digestive tract, it takes thousands of high-quality pictures, which are transmitted wirelessly to a receiver that is worn around the waist or carried in a small bag. The images are then uploaded to a computer, where they can be analyzed by a healthcare provider to diagnose various gastrointestinal conditions, such as Crohn’s disease, celiac disease, tumours, and bleeding.
Before the procedure, you may be advised to follow specific preparation instructions, such as fasting and avoiding certain medications. You’ll be asked to wear comfortable clothing and to remain still during the procedure to ensure that the capsule moves through the digestive system smoothly.
After the capsule is swallowed, you can resume their normal activities but may advised to avoid strenuous exercise, MRI scans, and high-voltage electrical devices until the capsule is eliminated from their body, which usually occurs within a few days. Your healthcare provider will provide instructions on how to return the receiver and capsule for disposal.
Carcinoma
A carcinoma (kaa-suh-now-muh)is cancer that begins in a tissue that lines the inner or outer surfaces of the body, the epithelial tissue, which is the lining of organs and other structures in the body. Carcinomas can occur in various parts of the body, such as the skin, appendix, and colon, among others.
CEA - carcinoembryonic antigen
Associated with the spread of tumour in the body cavity CEA (car-sin-o-em-bre-ON-ic an-tuh-jin) is a protein that is normally not detected in the blood of a healthy person. When certain types of cancer are present, CEA may be produced by the cancer cells. CEA may then be detected in blood, but it will not indicate which kind of cancer is present.
CEA is often used to monitor patients with cancers of the gastrointestinal (GI) tract such as bowel (colorectal) cancer. It may be raised in other cancers, such as ovarian and breast cancers, but can also be raised in benign conditions such as liver disease and inflammatory bowel disease (Crohns disease or ulcerative colitis).
It can also be high in heavy smokers and for other reasons.
Chemotherapy
Chemotherapy is a type of cancer treatment using drugs to kill cancer cells and/or limit their growth. For appendix cancer patients, there are a number of ways that chemotherapy can be given. In addition to eh way that these drugs are usually administered to the patient — by slow infusion into a vein and as tablets orally — appendix cancer and PMP patients often receive heated intraperitoneal chemotherapy (HIPEC) and/or EPIC (intraperitoneal chemotherapy).
Chemo Wash
The term “chemo wash” refers to a medical procedure called intraperitoneal chemotherapy (IP chemotherapy) or intraperitoneal hyperthermic chemotherapy (HIPEC), which is used in the treatment of advanced abdominal cancers, including appendiceal cancer and pseudomyxoma peritonei.
See HIPEC for more details.
#ChemoWash, #HIPEC, #HIPECprocedure, #HIPECsurgery
Cholecystectomy
A cholecystectomy is a surgical procedure to remove the gallbladder, which is an organ located near the liver that stores bile produced by the liver. The bile helps with the digestion of fats in the small intestine. The procedure is pronounced as “koh-luh-sis-TEK-tuh-mee”.
Colectomy
A colectomy is a surgical procedure to remove all or part of the colon (large intestine). It can be pronounced as “koh-lek-tuh-mee“.
Complete cytoreduction
Complete cytoreduction is the complete surgical tumour removal. This is a long operation which takes about 10 hours to complete and includes:
- removal of the right hemicolon
- spleen
- gall bladder
- greater omentum and lesser omentum
- stripping of the peritoneum from the pelvis and diaphragms
- tripping of tumour from the surface of the liver
- removal of the uterus and ovaries in women
- removal of the rectum in some cases
This is also referred to as a full peritonectomy. The goal is to remove tumour nodules down to 2.5mm.
Completeness of Cytoreduction (CC) score
The Completeness of Cytoreduction (CC) score is a scoring system used to evaluate the extent of surgery needed to remove pseudomyxoma peritonei (PMP).
The CC score ranges from 0 to 3, with 0 being no visible evidence of PMP and 3 indicating that there is extensive residual disease. The goal of surgery for PMP is to achieve a CC-0 or CC-1 score, which means that there is no visible evidence of cancer or only minimal residual disease remaining. Achieving a CC-0 or CC-1 score has been shown to improve survival rates and reduce the likelihood of recurrence.
The CC score is determined by the surgeon during the operation, based on the amount of tumour remaining after resection. The CC score is an important factor in determining the prognosis for PMP and can help guide treatment decisions, including the need for additional chemotherapy or other therapies.
CT Scan
A CT scan is used for diagnostic purposes. It’s a form of radiography in which your organs are scanned with X-rays and the results are put together by a computer to generate images of parts of the body. PMP patients usually have a chest, abdomen and pelvis CT.
Instructions you will be given for your CT scan will depend on where you have it done – the sensitivity of the scanning machines is different so what you need to do beforehand and what will happen on the day will vary.
D-J
DPAM
Formerly disseminated peritoneal adenomucinosis
The least-aggressive and least-invasive type of appendix cancer which it has spread (disseminated) throughout the abdomen (peritoneal cavity). These cancerous cells divide quickly and so do not to respond to systemic chemo. There is usually lots of mucin (musinosis) with adenomucinosis. This term is generally outdated.
Dysplasia
Dysplasia is a description of cells that look abnormal under the microscope but are not cancerous.
Endoscopy
Endoscopy is a procedure where a doctor puts a tube-like instrument into the body to look inside it. There
are many types of endoscopy, each of which is designed for looking at a certain part of the body. PMP patients will most frequently have a a colonoscopy (a look at the inside of the colon) or a sigmoidoscopy (a look at the sigmoid colon, the bit of your colon before your rectum and anus).
EPIC
EPIC is an abbreviation for “early postoperative intraperitoneal chemotherapy“. It is a treatment method used in combination with cytoreductive surgery for patients with pseudomyxoma peritonei. After removing all visible tumours, chemotherapy is administered directly into the peritoneal cavity (the space within the abdomen that contains organs such as the stomach and intestines) to target any remaining cancer cells. The goal of EPIC is to eliminate any microscopic residual disease that may be left after surgery and prevent recurrence of the cancer.
EPIC may the administered for a number of days (say 3 or 4) after surgery. It is also used to refer to the administration of chemotherapy directly into the abdomen following surgery as an alternative to HIPEC.
Fluoropyrimidine
Fluoropyrimidine is one of a group of substances used to treat cancer. A fluoropyrimidine is a type of antimetabolite – antimetabolites can have toxic effects on cells, such as halting cell growth and cell division.
Fluoropyrimidines used to treat appendix cancer and pseudomxoma peritonei include are capecitabine, floxuridine, and fluorouracil (5-FU).
Gastroscopy
A gastroscopy, also known as an upper endoscopy, is a medical procedure used to examine the inside of the upper gastrointestinal (GI) tract, including the esophagus, stomach, and duodenum (the first part of the small intestine).
During the procedure, a gastroenterologist, a specialist in digestive disorders, uses a flexible, thin, and lighted instrument called an endoscope to view the inside of your upper GI tract. The endoscope is inserted through the mouth and passed down the throat and esophagus to reach the stomach and duodenum. The endoscope has a camera at its tip, which captures images of the digestive tract and transmits them to a monitor for the gastroenterologist to view.
The purpose of a gastroscopy is to diagnose and treat various conditions of the upper GI tract, such as ulcers, inflammation, bleeding, and tumours. The procedure can also be used to take tissue samples (biopsy) for further examination, remove polyps or foreign objects, and perform certain therapeutic procedures.
Gastroscopy is typically performed under sedation or anesthesia to minimize discomfort and ensure patient safety. Before the procedure, you may be advised to follow specific preparation instructions, such as fasting, avoiding certain medications, and informing the healthcare provider of any medical conditions or allergies.
After the gastroscopy, you may experience some mild side effects, such as throat soreness, bloating, and mild cramping. These symptoms usually resolve within a few hours to a day. The gastroenterologist will provide instructions on when to resume normal activities, when to take any prescribed medications, and when to seek medical attention if complications occur.
GIST
Gastrointestinal stromal tumour (GIST) of the appendix is an extremely rare type of cancer that starts in the appendix, a small organ attached to the large intestine. GISTs are tumours that arise from specialized cells in the digestive system called interstitial cells of Cajal*, which help regulate digestive function.
GISTs can cause symptoms such as abdominal pain, nausea, vomiting, and changes in bowel habits. Treatment typically involves surgery to remove the tumour and any affected surrounding tissue, followed by targeted therapy with drugs that specifically target the abnormal proteins that are driving the growth of the tumour.
The prognosis for GISTs of the appendix varies depending on the stage of the tumour, but early diagnosis and treatment can improve outcomes. It is important to consult a doctor if you experience any persistent or unusual symptoms, as early diagnosis and treatment can be crucial in fighting this type of cancer.
*Interstitial cells of Cajal (ICC) are specialized cells found in the digestive system that help to regulate the muscular contractions that move food through the digestive tract. ICC are often referred to as the “pacemaker cells” of the digestive system, as they generate electrical signals that help to coordinate and synchronize the rhythmic contractions of the smooth muscle that lines the digestive organs.
ICC are found throughout the digestive system, from the esophagus to the rectum, and they play a critical role in maintaining normal digestive function. Abnormalities in ICC have been linked to a number of digestive disorders, including gastroparesis, chronic constipation, and certain types of cancer such as gastrointestinal stromal tumours (GISTs).
Goblet Cell
Goblet cell adenocarcinoma of the appendix is a rare and aggressive type of cancer that originates from the appendix, a small organ attached to the large intestine. This type of cancer is also known as mucinous adenocarcinoma of the appendix, since it arises from the mucous-producing goblet cells lining the appendix.The name goblet cell refers to the shape of the cells as they appear under a microscope – they are shaped like wine goblets.
Medical professionals have had a hard time understanding this rare type of cancer that starts in the appendix because there have been many different names for it. This has caused confusion about how serious the cancer is and how to treat it. But now there is a new approach recommended by the World Health Organization that should make it easier to understand and treat this cancer. By following these recommendations, medical professionals will be able to communicate better about the cancer and improve the chances of treating it successfully.
HAMN
High-grade appendiceal mucinous neoplasm (HAMN) is a rare type of tumour that arises from the appendix. It is considered to be an aggressive form of cancer that can spread to the surface of other organs and tissues within the abdomen. Unlike low-grade appendiceal mucinous neoplasms (LAMNs), HAMNs have a higher likelihood of metastasis and are more likely to invade surrounding tissues.
HAMNs are characterized by the presence of abnormal cells that are highly malignant and tend to grow rapidly. They typically present as a large tumour mass that is associated with symptoms such as abdominal pain, bloating, and nausea. HAMNs can also cause a buildup of mucus in the abdomen, which can lead to a condition known as pseudomyxoma peritonei.
HIPEC
Hyperthermic Intraperitoneal Chemotherapy
Heated chemotherapy, delivered directly into the abdomen, after complete cytoreduction. If the surgeons are able to remove the all the tumours, you may be given HIPEC.
Hyperthermic means that the chemotherapy solution used during the procedure is heated to a higher-than-normal temperature, typically around 41-43°C (105.8-109.4°F). This is usually Mitomycin C. This is put directly in your abdomen while you are in theatre. This elevated temperature is maintained throughout the duration of the procedure, usually around 90 minutes, to enhance the effectiveness of the chemotherapy drugs and to target cancer cells in the abdominal cavity. HIPEC will penetrate tumour nodules up to 2.5mm in size. The combination of chemotherapy drugs and hyperthermia can help to destroy cancer cells (increased cytotoxicity) while minimizing damage to healthy tissue.
Chemotherapy given into the abdomen during surgery is called intraoperative chemotherapy.
HITOC
Hyperthermic Intrathoracic Chemotherapy (HITOC) is a specialized medical procedure that involves delivering chemotherapy drugs directly to the thorax (chest) while the patient is under general anesthesia. The drugs are heated to a temperature of around 42°C, which is thought to enhance their effictiveness in killing cancer cells.
Hysterosalpingogram
A hysterosalpingogram (HSG) is a medical imaging procedure used to examine the uterus and fallopian tubes. It involves injecting a special dye into the uterus and taking X-ray images to evaluate the structure and function of the reproductive organs.
After the procedure, you may experience mild cramping, spotting, or discomfort. Over-the-counter pain medications can help relieve these symptoms. You may be advised to avoid sexual intercourse or using tampons for a few days after the procedure to reduce the risk of infection.
IPHP
Intraperitoneal hyperthermic perfusion (IPHP) is the same as HIPEC (Hyperthermic Intraperitoneal Chemotherapy).
Ileostomy
An ileostomy is a surgical procedure that involves creating an opening in the abdomen through which the end of the small intestine, called the ileum, is brought to the surface of the skin. The portion of the intestine that is brought to the surface is called a stoma. The stoma allows faeces to pass out of the body and into a collection bag that is attached to the skin.
Ileostomy is usually performed when the large intestine (colon) is not working properly, such as in cases of inflammatory bowel disease, bowel obstruction, or cancer. By diverting the fecal matter through the stoma, an ileostomy can help relieve symptoms such as abdominal pain, cramping, and diarrhoea. The procedure may be temporary or permanent, depending on the underlying condition and the patient’s individual circumstances.
#ileostomy
Intravenous
Intravenous (IV) means into or within a vein. Intravenous usually refers to giving a drug or other substance through a needle or tube inserted into a vein.
Jelly belly cancer
“Jelly belly” is a colloquial term used to describe pseudomyxoma peritonei (PMP), a rare form of cancer that starts in the appendix, and sometimes more rarely in other organs, and spreads to the abdominal cavity. PMP is characterized by the buildup of mucus-secreting tumours in the abdomen, which can cause the belly to become distended and swollen, leading to the “jelly belly” appearance. PMP is a slow-growing cancer and may not show symptoms until the tumours are large enough to put pressure on other organs. The cause of PMP is not well understood, and it is often misdiagnosed due to its rarity and lack of awareness. Treatment usually involves surgery to remove the tumours and may be followed by chemotherapy.
K-N
K-RAS Mutation
Our body is made up of tiny building blocks called cells, and they contain information called genes that tell the cells what to do. One of the genes is called the K-RAS gene, which gives instructions for making a protein that helps the cell grow and divide in a controlled way.
Sometimes, a mistake happens in the K-RAS gene that causes it to change in a way that affects how the protein works. This change is called a K-RAS mutation, and it can make the protein work too hard or too fast, leading to uncontrolled growth of the cell. When this happens, it can cause the cell to become cancerous and grow out of control.
K-RAS mutations are commonly found in many types of cancer, including lung cancer, pancreatic cancer, and colorectal cancer. They can be caused by things like smoking or exposure to certain chemicals, but sometimes they happen for no apparent reason. Scientists are working on ways to develop treatments that target K-RAS mutations to help fight cancer.
LAMN
LAMN, or low-grade appendiceal mucinous neoplasm, is a type of tumour that can develop in the appendix. It is a slow-growing tumour that can sometimes produce mucin, leading to a condition called pseudomyxoma peritonei. LAMN is considered a premalignant condition, which means it has the potential to develop into cancer, but it is not yet cancerous.
LAMN is often discovered incidentally during an appendectomy, which is the surgical removal of the appendix. Once diagnosed, patients with LAMN are usually closely monitored with regular follow-up appointments and imaging tests to check for any signs of progression. In some cases, further treatment such as a right hemicolectomy, which is the surgical removal of part of the colon, may be recommended to prevent the development of pseudomyxoma peritonei.
L-CRS
Laparoscopic cytoreductive surgery (L-CRS) is a minimally invasive surgical technique used to treat pseudomyxoma peritonei (PMP). The goal of L-CRS is to remove as much of the tumour tissue as possible from the abdominal cavity, while preserving healthy organs and tissues.
During L-CRS, a surgeon makes several small incisions in the abdomen and inserts a laparoscope, which is a thin tube with a camera and light attached. This allows the surgeon to see inside the abdominal cavity and identify the locations of the tumour tissue. The surgeon then uses specialized instruments to remove the tumour tissue, while leaving healthy organs and tissues intact.
L-CRS may be used alone or in combination with other treatments, such as hyperthermic intraperitoneal chemotherapy (HIPEC). Compared to traditional open surgery, L-CRS is associated with less pain, shorter hospital stays, and faster recovery times. However, not all patients with PMP are candidates for L-CRS, and the decision to pursue this treatment approach should be made in consultation with a team of medical professionals who specialize in treating the disease.
Lesion
Anything abnormal on or in the body, not just neoplasms.
In the context of pseudomyxoma peritonei (PMP), a lesion refers to an abnormal growth or tumour that develops on the peritoneum, which is the thin membrane that lines the abdominal cavity. These lesions are typically caused by the accumulation of mucinous fluid that is produced by the tumour cells and can vary in size and location. PMP lesions may be identified during diagnostic imaging tests, such as CT or MRI scans, and are often a key factor in determining the stage and severity of the disease. Treatment for PMP typically involves the removal of these lesions through surgery, which may be accompanied by hyperthermic intraperioneal chemotherapy (HIPEC).
Lynch syndrome
Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is an inherited genetic condition that increases the risk of developing certain types of cancer, particularly colorectal cancer, endometrial cancer, and other types of cancer such as ovarian, stomach, pancreatic, and urinary tract cancer. iIt s the most common cause of hereditary bowel cancer.However, not everyone with Lynch syndrome will get cancer.
Lynch syndrome is caused by mutations in genes that normally help repair DNA damage in cells, particularly in genes called MLH1, MSH2, MSH6, PMS2, and EPCAM. These mutations can interfere with the cell’s ability to repair DNA damage, leading to an increased risk of cancer.
Individuals with Lynch syndrome have a 50-80% lifetime risk of developing colorectal cancer, and an increased risk of developing other cancers as well. Each child of an affected parent has a 50% chance of inheriting the mutation.
Diagnosis of Lynch syndrome may involve genetic testing to identify mutations in the relevant genes, as well as regular screenings and surveillance to monitor for the development of cancer. Management and treatment of Lynch syndrome may involve regular colonoscopies and other screenings, prophylactic surgeries, and other interventions to help reduce the risk of cancer and manage the condition.
Malignant
Can spread to distant parts of the body.
MCP-H
high-grade mucinous carcinoma peritonei
Moderately or poorly differentiated adenocarcinomas
MCP-L
low-grade mucinous carcinoma peritonei
Low grade mucin producing disease including appendiceal adenoma, well-differentiated mucinous carcinomatosis, well-differentiated variants of mucinous adenocarcinomas.
Mitotic rate
Mitotic rate is a measurement of the number of cells undergoing mitosis, which is the process of cell division, i.e., how quickly cells are dividing.
In the context of cancer diagnosis and prognosis, mitotic rate is an important factor that is used to determine the rate of cancer cell growth and the aggressiveness of the cancer.
A high mitotic rate typically indicates that cancer cells are dividing rapidly and frequently, which can contribute to the growth and spread of the cancer. Conversely, a low mitotic rate may suggest that cancer cells are dividing more slowly, which can be a sign that the cancer is less aggressive and may respond better to treatment.
Mitotic rate is often determined by examining cancer tissue samples under a microscope, where the number of cells undergoing mitosis can be counted and recorded. This information can be used in conjunction with other factors, such as tumour size, grade, and stage, to develop a more complete picture of the cancer and its potential impact on the patient.
Mitotic rate can also be used to help guide treatment decisions, as cancers with a high mitotic rate may require more aggressive therapies to slow or stop the growth of cancer cells. In some cases, the mitotic rate may be used to predict the likelihood of cancer recurrence or the overall prognosis for the patient.
MOAS
"Mother of all Surgeries"
This is a nickname for the big cytoreductive surgery - full peritonectomy and HIPEC. It was thought up by the wife of an appendix cancer patient some years ago on her blog.
Mucinous appendiceal neoplasms
Mucinous appendiceal neoplasms are a type of cancer that starts in the appendix, a small organ attached to the large intestine. These tumours are called “mucinous” because they are made up of cells that produce a lot of mucus, a sticky substance that helps protect and lubricate the digestive system.
Mucinous appendiceal neoplasms can cause a variety of symptoms, such as abdominal pain, bloating, and changes in bowel habits. Treatment typically involves surgery to remove the appendix and any affected surrounding tissue, followed by chemotherapy if necessary.
The prognosis for mucinous appendiceal neoplasms depends on the stage of the cancer and other factors, but early detection and treatment can improve outcomes. It is important to consult a doctor if you experience any persistent or unusual symptoms.
NED
No Evidence of Disease
This is the term used when there are no signs of cancer in your body at a given time.
NG Tube
Nasogastric tube
A narrow tube which is passed through the bose into the stomach. It is usually then taped to your nose. It can be used to aspirate (to remove fluid) from your stomach after surgery or to administer nutition directly to the stomach (enteral nutrition).
Non-mucinous appendix adenocarcinomas
Non-mucinous appendix adenocarcinomas are a rare type of cancer that starts in the appendix, a small organ attached to the large intestine. Unlike mucinous adenocarcinomas, which are made up of cells that produce a lot of mucus, non-mucinous adenocarcinomas are made up of cells that do not produce mucus.
Non-mucinous appendix adenocarcinomas can cause a variety of symptoms, such as abdominal pain, bloating, and changes in bowel habits. Treatment typically involves surgery to remove the appendix and any affected surrounding tissue, followed by chemotherapy if necessary.
O-P
Oxaliplatin
Oxaliplatin is a type of chemotherapy drug that is used in the treatment of several types of cancer, including colorectal cancer, pancreatic cancer, and appendix cancer. It is also sometimes used in the treatment of appendix cancer. Oxaliplatin is one of a group of drugs called alkylating agents, which is a type of chemotherapy.
Oxaliplatin is one of several chemotherapy drugs that may be used in the treatment of appendix cancer. It works by interfering with the DNA in cancer cells, preventing them from dividing and growing. The drug is typically given intravenously, often in combination with other chemotherapy drugs. You pronounce oxaliplatin as ‘ox-ali-pla-tin’.
Like all chemotherapy drugs, oxaliplatin can have side effects, including fatigue, nausea, vomiting, diarrhea, and decreased blood cell counts. In some cases, it can also cause peripheral neuropathy, a type of nerve damage that can cause numbness, tingling, and pain in the hands and feet.
Overall, the effectiveness of oxaliplatin in treating appendix cancer depends on the individual case and other factors, such as the stage and extent of the cancer. Your healthcare provider can help determine if chemotherapy is the most appropriate treatment for your particular case.
Parietal Peritoneum
The parietal peritoneum is the outer layer of the peritoneum, which is a serous membrane that lines the abdominal cavity and covers many of the abdominal organs. It is also known as the parietal layer of the peritoneum. The parietal peritoneum is attached to the abdominal wall and the pelvic cavity, and it provides support and protection to the internal organs. It also helps to produce and absorb peritoneal fluid, which acts as a lubricant and helps to reduce friction between the abdominal organs during movement. The parietal peritoneum is sensitive to pain, which allows for the perception of abdominal pain or discomfort.
Partial Gastrectomy
A partial gastrectomy is a type of surgery that doctors do to remove a part of the stomach. They do this when someone has a problem with their stomach, like a tumour or a hole in it, and they need to take out that part to make the person feel better. After the surgery, the person’s stomach will be smaller, so they may need to eat smaller meals and more frequently. But with time and care, the person can still have a normal life.
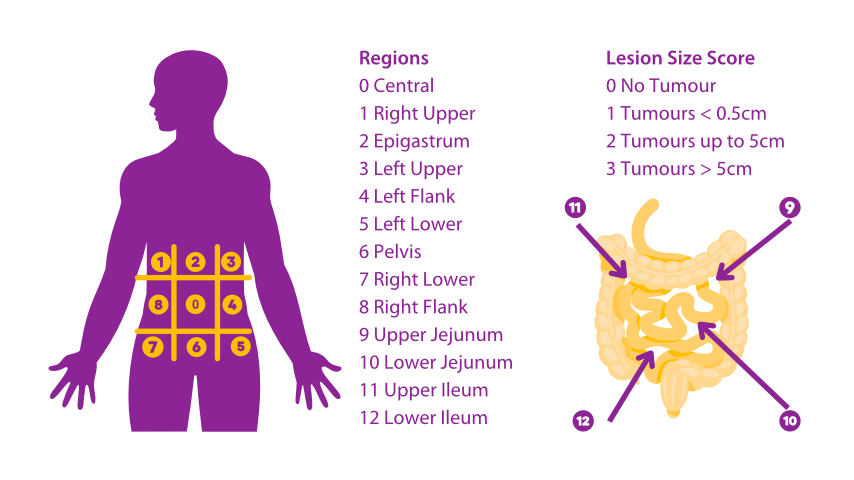
PCI Score
The Peritoneal Cancer Index (PCI) is a scoring system used by surgeons to assess the extent of peritoneal cancer. It is a numerical score that ranges from 0 to 39, with higher scores indicating more advanced disease.
During surgery, the abdomen is divided into different regions, and the surgeon assigns a score of 0 to 3 for each region based on the amount and size of cancer nodules present. A score of 0 means no cancer is present, while a score of 3 means that the region is completely covered in cancer nodules. The scores for all regions are added together to calculate the final PCI score.
The PCI score is important because it helps the surgeon determine the feasibility of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). A PCI score of 20 or less is generally considered favorable for CRS and HIPEC, while scores higher than 20 may indicate a poorer prognosis and may require alternative treatments.
The PCI scoring system is widely used in the evaluation and treatment of peritoneal surface malignancies, particularly in the context of pseudomyxoma peritonei and appendix cancer.
Peritoneal Mesothelioma
Peritoneal Mesothelioma (also referred to as malignant peritoneal mesothelioma, peritoneal malignant mesothelioma, malignant primary peritoneal mesothelioma and abdominal mesothelioma) is a rare, usually aggressive, form of cancer affecting the serosal (inner) surface of the peritoneum.
Peritoneal Surface Malignancies
Rare peritoneal surface malignancies are a group of rare cancers that develop on the surface of the peritoneum, which is the membrane lining the abdominal cavity. These cancers can originate from various organs within the abdomen, including the appendix, colon, rectum, ovary, stomach, and others. Examples of rare peritoneal a surface malignancies include pseudomyxoma peritonei, peritoneal mesothelioma, and gastrointestinal stromal tumours. Due to their rarity and complexity, the treatment of these cancers typically involves a multidisciplinary approach and specialized centers with expertise in peritoneal surface malignancies.
Cytoreductive surgery and HIPEC (hyperthermic intraperitoneal chemotherapy) are often used together to treat peritoneal surface malignancies, including peritoneal mesothelioma and pseudomyxoma peritonei.
Cytoreductive surgery involves removing as much of the visible tumour as possible through surgery. This may include removing parts of organs, tissues, or the entire peritoneal lining. The goal is to reduce the amount of tumour present in the abdomen to the point where the remaining tumour cells can be effectively treated with chemotherapy.
After the cytoreductive surgery is complete, HIPEC is administered. This involves bathing the abdominal cavity with a heated chemotherapy solution for several hours. The heat of the solution increases the effectiveness of the chemotherapy, and because it is administered directly into the abdominal cavity, it can target any remaining cancer cells that were not removed during the surgery.
Together, cytoreductive surgery and HIPEC offer a potentially curative treatment option for patients with peritoneal surface malignancies. However, not all patients are suitable candidates for this treatment and the decision to pursue this treatment should be made on a case-by-case basis by a team of medical professionals experienced in treating these types of cancers.
Peritonectomy
A peritonectomy is a surgical procedure to remove part or all of the peritoneum, the membrane that lines the abdominal cavity. It is pronounced as “peh-rih-tuh-NEK-tuh-mee”.
Peritoneum
The peritoneum is the tissue that lines your abdominal wall and covers most of the organs in your abdomen.
PIPAC
PIPAC stands for Pressure-Controlled Intermittent Positive-Pressure Aerosol Chemotherapy. It is a specialized medical procedure that involves delivering chemotherapy directly to the abdominal cavity using a combination of pressure and aerosol.
During PIPAC, a small, specialized device is used to deliver a mist of chemotherapy drugs directly into the abdominal cavity. The pressure is controlled to ensure that the drugs reach all areas of the abdomen and peritoneal cavity. This allows for higher doses of chemotherapy to be delivered directly to the site of the cancer, while minimizing side effects to other parts of the body.
PIPAC is typically used to treat cancers that have spread to the peritoneal cavity, such as pseudomyxoma peritonei (PMP), and is performed in conjunction with other treatments such as surgery and systemic chemotherapy. Your doctor can provide more information on whether PIPAC is a suitable treatment option for your specific case.
PITAC
Low-dose Pressurized Intrathoracic Aerosol Chemotherapy (PITAC) is a specialized medical procedure that involves delivering low doses of chemotherapy drugs directly to the thorax (chest) using a pressurized aerosol system. The purpose of PITAC is to deliver the chemotherapy drugs directly to the cancer cells in the chest, while minimizing exposure of other parts of the body to the drugs.
Polyp
A polyp is a growth that protrude from a mucous membrane.
When polyps are attached to the mucous membrane by a thin stalk they are called pendunculated polyps; if no stalk is present, they are sessile polyps.
PRGS
The peritoneal regression grading score (PRGS) is a grading system used to evaluate the effectiveness of treatment for peritoneal surface malignancies such as pseudomyxoma peritonei. It is a four-tiered scoring system that assesses the extent of peritoneal disease and the degree of response to treatment. The score is based on four criteria:
- the size and extent of the tumour nodules,
- the degree of fibrosis or scarring,
- the amount of ascites or fluid in the abdominal cavity, and
- the presence of mucus.
The PRGS score ranges from 0 (no evidence of disease) to 3 (significant residual disease). A lower PRGS score indicates a better response to treatment and improved patient outcomes.
Proctectomy
A proctectomy is a surgical procedure to remove all or part of the rectum. The term proctectomy is pronounced as “prok-tek-tuh-mee“.
pseudomyxoma peritonei
Pseudomyxoma peritonei or PMP
“Pseudomyxoma peritonei” literally means “false mucinous tumour in the abdomen”. In the 1860s, the first mucinous tumours were discovered in the chest, surrounding the heart. Doctors called them “myxomas.” When a surgeon found a mucinous tumour in the abdomen twenty years later, he called it a “pseudomyxoma” (false myxoma), because the chest tumours were discovered first.
This phrase is sometimes used to refer to all types of appendix cancer. It is sometimes used to refer to the mucin only, or to the less-aggressive form of appendix cancer.
Q-Z
Right hemicolectomy
A right hemicolectomy is a surgical procedure that involves the removal of the right side of the colon (large intestine). This procedure is usually performed to treat conditions such as appendix cancer, pseudomyxoma peritonei, Crohn’s disease, and ulcerative colitis.
The right side of the colon, including the caecum, ascending colon, and part of the transverse colon, is removed. The remaining part of the colon is then reconnected to the small intestine, allowing for the normal passage of stool.
You may need to follow a special diet and take medications to prevent complications.
Recurrence
Recurrence is used to describe cancer that has come back, usually after a period of time during which the cancer or disease was not present or could not be detected (no evidence of disease). This can also be called recurrent
cancer or disease.
Signet Ring
The name signet cell tumours comes from the appearance of the cells under a microscope; signet ring cells resemble signet rings.
Shake and Bake
“Shake and Bake” is a slang term used to describe the combination of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) used to treat pseudomyxoma peritonei (PMP). PMP is a rare type of cancer that originates in the appendix and can spread throughout the abdominal cavity, causing a buildup of mucinous fluid.
The Shake and Bake procedure involves the surgical removal of all visible tumour tissue in the abdominal cavity (cytoreductive surgery) followed by the administration of heated chemotherapy drugs directly into the abdominal cavity (hyperthermic intraperitoneal chemotherapy). The chemotherapy drugs are heated to a temperature of around 41-43°C (105.8-109.4°F) to enhance their effectiveness.
The Shake and Bake procedure is named after the cooking method of the same name, in which food is placed in a bag and shaken to coat it in a mixture of flour and seasonings before being baked.
HIPEC has been shown to improve survival rates for PMP patients, and the Shake and Bake approach is a highly specialized and complex surgery that is only performed by a small number of experienced surgical teams around the world.
While the Shake and Bake procedure can be highly effective in treating PMP, it is also a major surgery with significant risks and potential complications, and is not appropriate for all patients. Each case is evaluated on an individual basis to determine if the procedure is suitable and if the potential benefits outweigh the risks.
SBO
Small Bowel Obstruction
A small bowel obstruction is an obstruction of the small bowel which means the small bowel effectively becomes blocked. There can be a number of causes for this with the main one being adhesions following surgery.
Small Bowel Obstruction
A small bowel obstruction (SBO) occurs when the small intestine is partially or completely blocked, which can prevent the normal passage of food, fluid, and gas through the digestive tract. This can cause symptoms such as abdominal pain, bloating, nau sea, vomiting, and constipation. Common causes of small bowel obstruction include adhesions (scar tissue), hernias, tumours, and inflammation. Treatment typically involves bowel rest, hydration, and sometimes the use of a nasogastric tube to relieve pressure and reduce symptoms. In some cases, surgery may be necessary to remove the obstruction or repair the underlying cause.
Splenectomy
A splenectomy is a surgical procedure to remove your spleen. It is pronounced as “spleh-NEK-tuh-mee”.
Stoma
A stoma is a special opening that doctors make in a person’s belly. This opening is made from a part of the person’s intestine, and it’s brought outside the body so that poop can come out into a special bag that sticks to the person’s belly. It’s kind of like a new way for the poop to get out of the body when the normal way doesn’t work well.
A stoma can be created from the small intestine or colon, and is brought through the abdominal wall and attached to a bag or pouch. This bag or pouch is worn outside of the body and collects the waste products, which can then be emptied and replaced as needed. A stoma can be temporary or permanent, and may be created for various conditions including pseudomyxoma peritonei and appendix cancer.
The Sugarbaker Technique
The Sugarbaker technique was developed by Paul Sugarbaker at the Washington Cancer Institute. It involves complete surgical tumour removal combined with intraoperative heated chemotherapy, followed by postoperative intraperitoneal chemotherapy.
Survivor
When someone is diagnosed with cancer, they are called a cancer survivor for the rest of their life. This also includes their family, friends, and people who take care of them, because they are all affected by the experience.
TPN
Total Parenteral Nutrition
Parenteral Nutrition is the administration of nutrients intravenously. When this is the only source of nutrition, it is called Total Parenteral Nutrition or TPN. It is often given after surgery to allow the intestines to rest and contains a balance of carbohydrates, fats, minerals and vitamins.
Enteral nutrition is the delivery of balanced nutrition directly usually into the stomach but also to the duodenum.
Tumour
A mass due to autonomous growth of cells, whether benign or malignant.
Watch and wait
“Watch and wait” is a medical approach in which doctors closely monitor a patient’s condition, typically through regular imaging scans and blood tests, without immediately starting treatment. This approach is often used for patients with pseudomyxoma peritonei (PMP) who have small and slow-growing tumours that are not causing significant symptoms or complications.
During the watch and wait period, doctors will monitor the patient’s condition and may recommend treatment if there are any changes or signs that the cancer is progressing.
Watch and wait can be challenging for patients who may feel anxious or uncertain about not receiving immediate treatment for their cancer. However, for some patients with PMP, watch and wait can be a viable option that allows them to avoid the potential side effects of treatment and maintain a good quality of life.
Visceral Peritoneum
The visceral peritoneum is a thin, transparent layer of tissue that covers the organs in the abdominal cavity, such as the stomach, liver, and intestines. It is also known as the serosa. The visceral peritoneum provides a smooth surface that allows the organs to slide easily against one another and other abdominal structures. It also provides a protective layer and helps to prevent friction and damage to the organs. Blood vessels and nerves that supply the organs pass through the visceral peritoneum. The visceral peritoneum is one of two layers of peritoneum, the other being the parietal peritoneum, which lines the abdominal wall.
WOC/ET Nurse
A “WOC” (Wound, Ostomy and Continence) nurse, previously known as an “ET” (Enterostomal Therapy) nurse, is often the best medical professional for dealing with problems involving ostomies. These nurses are also often known as stoma care nurses or, more simply, stoma nurses.
Apply for a Great North Run 2024 place with Pseudomyxoma Survivor
Missed out on the ballot for the Royal Parks Half Marathon, presented by Royal Bank of Canada? Apply for a Pseudomyxoma Survivor charity place now!
Apply for a Great Birmingham 10k Run 2024 place with Pseudomyxoma Survivor
Join Team Pseudomyxoma Survivor and make strides against PMP and appendix cancers by securing your charity place in the Great Birmingham 10k.
Apply for a Great Scottish 10k Run 2024 place with Pseudomyxoma Survivor
Missed out on the ballot for the Royal Parks Half Marathon, presented by Royal Bank of Canada? Apply for a Pseudomyxoma Survivor charity place now!
References
Cancer Research UK
CRUK. Various. Cancer Research UK. Retrieved March 21, 2023, from https://www.cancerresearchuk.org/
Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique)
NICE. Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique). National Institute for Health and Care Excellence. Retrieved March 21, 2023, from https://www.nice.org.uk/guidance/ipg56
General Information
The peritonectomy unit at St George Hospital (n.d.). General Information. St. George Peritonectomy and Liver Cancer Unit. Retrieved March 21, 2023, from https://stgeorgeperitonectomy.com.au/for-patients/patient-information/general-information/
Macmillan Cancer Support
Macmillan Cancer Support. Various. Macmillan Cancer Support. Retrieved March 21, 2023, from https://www.macmillan.org.uk/
Merriam Webster
Merriam-Webster, Incorporated. Various. Merriam Webster. Retrieved March 21, 2023, from https://www.merriam-webster.com
National Cancer Institute
NIH Various. National Cancer Institute. Retrieved March 21, 2023, from https://www.cancer.gov/
Oxford Learner's Dictionary
Oxford University Press (n.d.). Various. Oxford Learner’s Dictionary. Retrieved March 21, 2023, from https://www.oxfordlearnersdictionaries.com
Technique of pressurized intrathoracic aerosol chemotherapy (PITAC) for malignant pleural effusion.
Drevet G, Maury JM, Bakrin N, Tronc F (2020). Technique of pressurized intrathoracic aerosol chemotherapy (PITAC) for malignant pleural effusion. Pleura Peritoneum. 2020;5(4):20200129. Published 2020 Nov 9. doi:10.1515/pp-2020-0129
Revised April 13, 2023.
Home > Frequently asked Questions