About
Pseudomyxoma
Peritonei
Information about PMP
What is pseudomyxoma peritonei?
Also known as PMP, pseudomyxoma peritonei is a rare cancer that generally starts in the appendix.
How can pseudomyxoma peritonei be diagnosed?
There are several tests and procedures that can help to diagnose or to rule out pseudomyxoma peritonei (PMP). Here, we look at some of them.
Where can I go for treatment?
Understand the options you have for treatment and where to find a pseudomyxoma peritonei/appendix cancer specialist.
Information about pseudomyxoma peritonei (PMP)
When you are newly diagnosed with PMP, it can be very confusing, almost bewildering. There are so many expressions to learn and options to understand. We’re here to help with that. Our information about pseudomyxoma peritonei is written by patients and reviewed by specialists. This gives you an insight from your point of view that you know is correct.
What is Pseudomyxoma Peritonei?
Pseudomyxoma peritonei is pronounced ‘sue-doh-mix-oh-muh pary-ih-ton-nee-i’ and is often abbreviated to PMP. It is an unusual condition in which a mucinous cancer spreads within the abdominal cavity causing mucin (mucus) to accumulate.
In most cases, this cancer starts in the appendix. More rarely, it can start in other parts of the body such as the bowel, an ovary or the bladder. It affects around two people per million each year of all ages, both men and women. A tumour develops in the appendix from a polyp which is a small growth on the inner lining of your appendix. At this early stage, the tumour is rarely discovered as it doesn’t cause any symptoms.
Left untreated, the tumour grows and eventually bursts through the wall of the appendix into your abdominal cavity where more tumours then develop. These tumours then secrete a jelly-like substance called mucin which accumulates in your abdominal cavity. It is this build up of mucin that causes symptoms, the abdomen swells leading to the characteristic ‘jelly belly’ and vital organs are compressed.
The abdominal cavity is also called the peritoneal cavity, because it is lined by a thin membrane called the peritoneum. This membrane covers the abdominal organs and the inside of the abdomen. The word peritonei reflects the fact that the peritoneum is involved in PMP.
Grade refers to the aggressiveness of a cancer. In PMP, high grade lesions tend to grow quickly and patients are more likely to be offered chemotherapy. Low grade lesions grow more slowly and sometimes may be present for years without causing serious problems.
Unfortunately, medical terms can sometimes be confusing and there are often multiple names for the same condition. PMP is no exception and has been classified in different ways over the years.
The current classification, endorsed by the World Health Organization (WHO) has three classifications of pseudomyxoma peritonei:
Low grade
Low grade mucinous carcinoma peritonei or MCP-1
High grade
High grade mucinous carcinoma peritonei or MCP-2
High grade with signet ring cells
High grade mucinous carcinoma peritonei with signet ring cells or MCP-3
PMP isn’t like other types of cancer that involve the abdomen in that it seldom spreads through the bloodstream or lymphatic system. It stays contained within the abdomen where it spreads along the inner surfaces, spread by the mucin. It isn’t currently known what causes PMP. The name ‘pseudomyxoma peritonei’ means “false mucinous tumour of the peritoneum”; the peritoneum is another name for your abdominal cavity.
Spotting the symptoms
Symptoms of pseudomyxoma peritonei usually take a while to appear. Some patients don’t show any symptoms for several years. As the symptoms of PMP vary widely among patients, it’s hard to say what to look for. As the disease progresses, many patients report:
- Abdominal swelling or an increase in abdominal girth
- Changes in bowel habit
- Loss of appetite
- Pelvic or abdominal pain
- General fatigue
- Bowel irritation
These symptoms can also be caused by lots of medical conditions other than PMP. However, due to the nature of this cancer, it’s vital to rule out pseudomyxoma peritonei as a cause. Any unexplained symptoms should always be discussed with your doctor.
The first sign for me was having what appeared as flu-like symptoms.
All my joints started to ache but within ten minutes of that I then had abdominal pain. I was then diagnosed with PMP two weeks later after my eighth day in hospital.
For 20 years as it grew I was told I was just fat and to exercise more for the fatigue.
I kept saying I didn’t eat enough to account for the rate of growth but nooo.
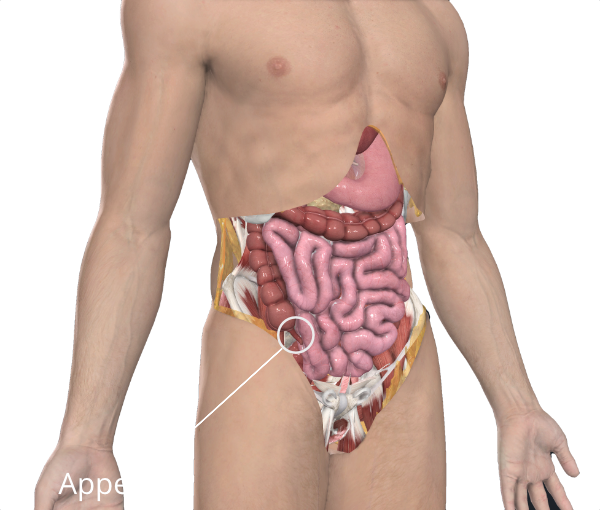
What is this appendix thing anyway?
Your appendix is on your right-hand side, just inside your hip and is a small tube, shaped like a worm. It’s about 10cm long, a bit longer than your finger. It’s attached to your large intestine (your colon) where it meets with your small intestine. It’s closed at one end and open where it connects to your intestines. Your appendix has a lining that produces mucus as does your small intestine. It can also contract like your small intestine, though unlike your intestines, food does not pass through it – there is nowhere for it to go. Your body produces mucus to protect the lining of the tubes in your body, including the intestines and appendix.
This mucus is made up of mucin and salts in water. The mucus is produced by a thin layer of epithelial cells that line the inside of your appendix and intestine. Until recently, it was thought that the appendix had no purpose – that it was a remnant that we had used in earlier times. Now it is thought to play a part in the immune system although it isn’t fully understood what that role is.
Your appendix is attached to your caecum, part of your colon. As a result, appendix cancer is considered a colorectal cancer although the standard of care for treatment is different to other colorectal cancers. Colorectal cancers are also part of a larger group of cancers of gastrointestinal tract, or GI, cancers.
Epithelial cells make up one of four tissue types in your body (the others are connective tissue, muscle tissue and nervous tissue). As well as lining the major cavities of your body and forming the structure of your lungs, epithelial cells line most organs including your stomach and your small intestine. You also have them inside your nose – you will be quite familiar with their ability to produce mucus if you have ever suffered from the common cold! Names are very confusing – the small intestine is sometimes called the small bowel. The large intestine is sometimes called the large bowel or the colon.
What treatment is available?
Treatment for mucinous tumors that have spread into the abdomen, either low grade or high grade, is cytoreductive (debulking) surgery to remove the mucin and tumour implants in the abdominal cavity. This is followed by intraoperative hyperthermic peritoneal chemotherapy (HIPEC). Early postoperative intraperitoneal chemotherapy (EPIC), in which chemotherapy liquid is put into the abdomen using a port or tube soon after the surgery is over, may also be used. The whole procedure is also called “the Sugarbaker technique”, after Dr Paul Sugarbaker. That’s a lot of terms!
Cytoreductive surgery is an operation that removes the tumours that have seeded around the abdominal cavity. It is a very long operation – usually between 10 and 14 hours. The surgeons work to remove all visible tumours in your abdominal cavity, that’s down to 2mm. HIPEC is liquid chemotherapy solution that is poured directly into the abdominal cavity at the end of the operation. The aim of this is to kill off any remaining cancer cells after the operation to prevent them from growing new tumours. Chemotherapy solution is a liquid chemical solution that kills cancer cells. It is usually heated to about 42C (your body temperature is usually about 37C).
When the chemotherapy solution is heated, it is thought to be more effective in killing cancer cells. The liquid chemotherapy can reach more places in the abdominal cavity while it is still open. It is swished around and circulated inside you to reach areas where those cancer cells that are not visible to the naked eye are hiding. This is done for about 90 minutes (the time can be different). It is drained off and then you can be closed up. Just in case any of those cancer cells are still hiding in there, you may be given EPIC for several days in a row after your operation. Using a port into your abdominal cavity, the liquid chemotherapy is poured in and then drained out over a 24 hour period.
Why can’t I just have my appendix out?
You wouldn’t usually have any symptoms until the tumour has broken through the wall of the appendix and released mucinous cells into your abdominal cavity. Just having your appendix out at that stage wouldn’t remove those cells and tumours would continue to develop, mucin would continue to be produced and PMP would develop. For a low grade tumour that hasn’t ruptured and that is confined to the appendix, treatment would be removal of the appendix. When the appendix is removed, it should be contained in a plastic bag to avoid mucin and tumour cells spilling into the abdominal cavity. For a high grade tumour that hasn’t ruptured, treatment would be an appendectomy and right hemicolectomy (removal of the appendix and up to half of the right side of the colon).
I has no symptoms at all…
I developed an umbilical hernia and when it was being repaired they found the mucin. Only with follow up tests they found the root cause.
My only symptom was my abdomen was swelling at a fairly fast rate.
I looked eight months pregnant before surgery. My appendix had been ‘leaking’ into my abdomen and my ovary just grew and grew.
Frequently Asked Questions
My doctor has diagnosed appendix cancer, why do I need a second opinion?
If you have been diagnosed with appendix cancer, it is vital to seek a second opinion from an experienced physician who has seen and treated numerous cases of the disease.
Why is appendix cancer so difficult to diagnose?
Diagnosing appendix cancer can be difficult due to the lack of effective screening tests and the general nature of the symptoms.
Just how rare is PMP?
PMP is identified by Eurordis as a rare or “orphan” disease (one which affects less than 1 in 2000 people).
Where can I go for treatment?
In the UK, there’s two hospitals which are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of pseudomyxoma peritonei. These are the Basingstoke and North Hampshire Hospital and the Christie Hospital in Manchester. Both of these hospitals have an NHS Peritoneal Malignancy/Tumour team specialising in PMP. Both also see patients privately in separate clinics. The referral process to either Basingstoke or to the Christie depends on which part of the UK you live in.
For more details, and the contact details for both Basingstoke and the Christie, please visit our UK specialists page. We do hold information for other countries and we have this under constant monitoring to keep it as up to date as we can. If you need some help, get in touch. Pseudomyxoma Survivor doesn’t endorse any particular surgeon, specialist or cancer treatment centre. We simply share practical information and national guidelines.
What do you call that?
You may hear lots of terms, unfamiliar words which are difficult to remember. There is so much to take in and you won’t always have time to think to ask the right question. Our glossary is a place where you can look up exactly what something means.
References
A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia
Carr, Norman J. FRCPath; Cecil, Thomas D. MD; Mohamed, Faheez; Sobin, Leslie H.; Sugarbaker, Paul H.; González-Moreno, Santiago MD PhD; Taflampas, Panos MD; Chapman, Sara PhD; Moran, Brendan J. MD, A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia, The American Journal of Surgical Pathology: January 2016 – Volume 40 – Issue 1 – p 14-26 doi: 10.1097/PAS.0000000000000535
Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique)
National Institute for Health and Care Excellence (NICE) Complete cytoreduction for pseudomyxoma peritonei (Sugarbaker technique), April 2004 [Online]. Available https://www.nice.org.uk/Guidance/ipg56 [Accessed February 2018]. Under review February 2018.
Pseudomyxoma peritonei
Cancer Research UK, Pseudomyxoma peritonei, 2016 [Online]. Available http://www.cancerresearchuk.org/about-cancer/pseudomyxoma-peritonei [Accessed February 2018].
Pseudomyxoma peritonei (PMP)
Macmillan, Pseudomyxoma peritonei (PMP), 2016 [Online]. Available https://www.macmillan.org.uk/information-and-support/pseudomyxoma-peritonei-pmp [Accessed February 2018].